Vulval lichen sclerosus
What is lichen sclerosus?
Lichen sclerosus (‘like-en skler-oh-sus’) is a chronic (long-term) skin condition. It can cause inflammation, white patches, and scarring of the skin.
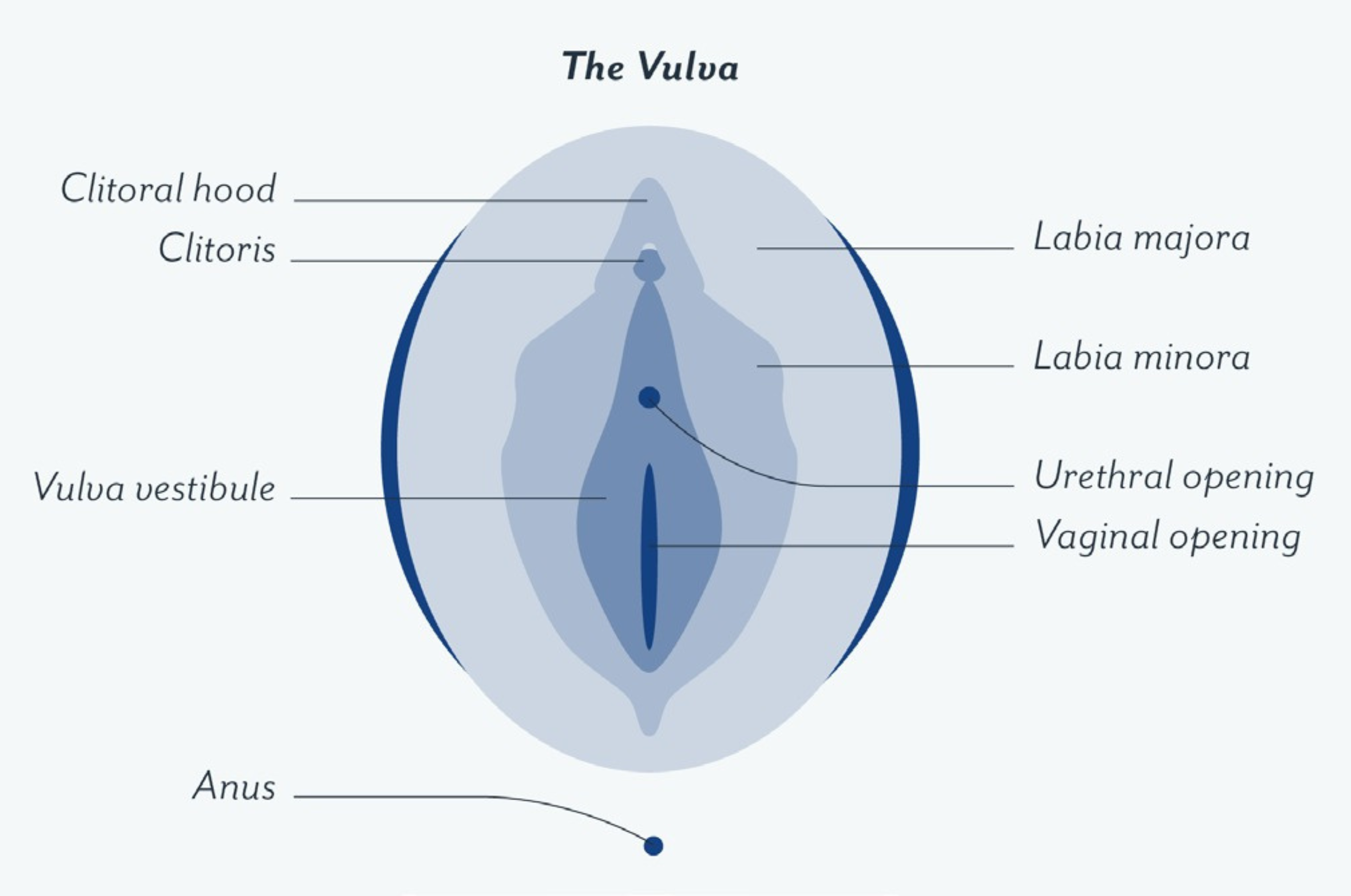
Lichen sclerosus can occur anywhere on the body but most often affects the skin around the vulva, penis, or anus.
Lichen sclerosus is more common in adults with a vulva. However, it can occasionally affect children or adults with a penis. It can occur at any age but is more common in people over 50.
Vulval lichen sclerosus is where the condition occurs in the vulval area. Lichen sclerosis does not affect the vagina because it is different tissue.
If vulval lichen sclerosus is left untreated for a long time, there can be an increased risk of vulval skin cancer.
What causes lichen sclerosus?
- The cause of vulval lichen sclerosus is not fully understood.
- Lichen scleosus is thought to have a genetic basis because it is more common in people who have a family member with the condition.
- It is sometimes classified as an autoimmune condition, where the body attacks its own cells by mistake.
- It can be associated with conditions related to the immune system, such as diabetes, coeliac disease, thyroid conditions, and pernicious anaemia.
- Lichen sclerosus is not an infection. It is not contagious, so you cannot pass it to a sexual partner.
What are the symptoms of lichen sclerosus?
Symptoms of vulval lichen sclerosus include:
- Itching of the vulval or anal area. The itching can always be present, or it can come and go. Itching is a common symptom. However, not everyone experiences it.
- Pale, white skin patches on the vulva that can sometimes look crinkled or thickened.
- Skin dryness.
- Soreness and burning of the vulva, particularly with sexual activity.
- Small cracks in the skin (fissures). These can occur because of scratching and can become very sore. It can become painful to urinate, and if fissures occur around the anus, there can be pain with bowel movements.
- White patches on the skin in other areas of the body can occur in about 1 in 10 people with vulval lichen sclerosus. The common sites for this are on the back, waist area, and under the breasts.
- About 1 in 10 people do not have symptoms, and the diagnosis is made when the affected area is examined for another reason.
- Chronic inflammation can cause scarring and changes to the vulva's appearance. These changes can include:
- Pale, white skin patches that can sometimes look crinkled but can also have a shiny, smooth surface. These can be individual patches or may involve the entire vulva, extending down to the skin around the anus.
- There may be white dots or small splotches on the skin.
- Some purplish/red areas or small red spots. These are bruises due to tiny areas of bleeding into the skin, often because of scratching.
- There may be changes to the vulval skin folds; the labia minora (inner lips) may become flattened, the vulval skin can close over the clitoris, and the skin at the entrance to the vagina may shrink, making it less flexible.
How is vulval lichen sclerosus diagnosed?
Healthcare providers familiar with the condition may diagnose vulval lichen sclerosus by looking at the skin of your vulva.
Your doctor may confirm the diagnosis by taking a skin biopsy. A biopsy is a simple procedure that involves numbing the skin with a local anaesthetic then removing a small piece of skin that is examined under the microscope.
How do you treat lichen sclerosus?
While there is no cure for lichen sclerosus, the symptoms can usually be controlled very well using steroid ointment or cream.
As vulval lichen sclerosus is a chronic (long-term) condition, this treatment needs to be long-term.
With proper treatment, you can expect excellent results. Inflammation will settle, symptoms will lessen, further scarring and damage will be prevented, and the appearance and texture of the vulval skin will improve. However, any changes to the skin, such as scarring and loss of tissue that has already occurred, cannot be reversed.
You can use steroid creams or ointments safely in the genital area. Your healthcare provider will instruct you on how to use it correctly. Treatment needs to be ongoing, and it is essential not to stop your treatment, as lichen sclerosus symptoms can recur or progress without it.
Skin irritation, like scratching, or infections such as yeast or bacteria can worsen lichen sclerosus. Therefore, it is important to avoid skin irritation as much as possible. Any infections from yeast or bacteria need to be treated early.
What happens if vulval lichen sclerosus is not treated?
- If it is not treated, vulval lichen sclerosus can cause significant problems and affect your quality of life.
- The changes to the vulva that occur, such as loss of tissue and scarring, are permanent and not reversible.
- Scarring can make penetrative sex uncomfortable, if not impossible, and passing urine may become difficult.
- Persistent discomfort in the vulval area can lead to a chronic pain condition in the long term.
- If lichen sclerosus is left untreated there is a 5% (1 in 20) chance of it progressing to cancer of the vulva. Ongoing treatment reduces this risk to less than 1%.
What can I do to help manage the symptoms?
As well as having treatment, there are a few things you can do to help manage the symptoms:
- Gently clean the vulva using only water over the skin surface and avoiding soap, gels, body wash etc.
- Use a simple, hypoallergenic moisturiser to relieve dryness and itching.
- Try to avoid tight clothing.
- You may need to avoid or decrease some activities which put pressure on the vulva, like bicycle or horse riding, that may worsen symptoms.
- If dryness is a problem, and you are around the age of menopause, ask your healthcare provider about using vaginal oestrogen cream or pessaries to help with this. Hormone replacement therapy may also be helpful.
- Avoid scratching when you are itchy. These are some things that may help:
- Distraction can be helpful. For example, if the itch becomes unbearable in bed, get up and find something to do that occupies your hands and attention.
- Keep your nails short so scratching in your sleep does not damage the skin.
- Taking an oral antihistamine at bedtime may also help to control the itching.
- Applying a cool pack applied to the vulva may be helpful.
Is it okay to have sex if I have vulval lichen sclerosis?
- It is safe to have sex. However, scarring can make the skin of the vulva tight and more likely to split, which can be painful. This includes the entrance to the vagina.
- Sex should be avoided if it is painful, as it can irritate the affected skin or cause small skin tears. It’s best to wait until your symptoms have improved to try any penetrative sex.
- If penetrative sex continues to be a bit painful, using a lubricant can help to make it more comfortable and reduce the risk of small skin tears.
- Talk to your doctor or a sexual counsellor about ways to manage painful sex or the fear of pain during sex. There are many ways to maintain intimacy and sexual closeness that do not involve penetrative sex.
- Dilators that can help open the entrance to the vagina and exercises that help relax the muscles of the pelvic floor can also be helpful. A sexual counsellor or pelvic health physiotherapist can help you with this.