Sexual and Reproductive Health Information
The information brochures below will help to answer all your sexual health and relationship wellbeing questions.
General Information
Enjoying Sex Safely
Cervical Screening
Human Papilloma Virus (HPV)
Early Pregnancy Health and Care
Pregnancy Options
Painful...
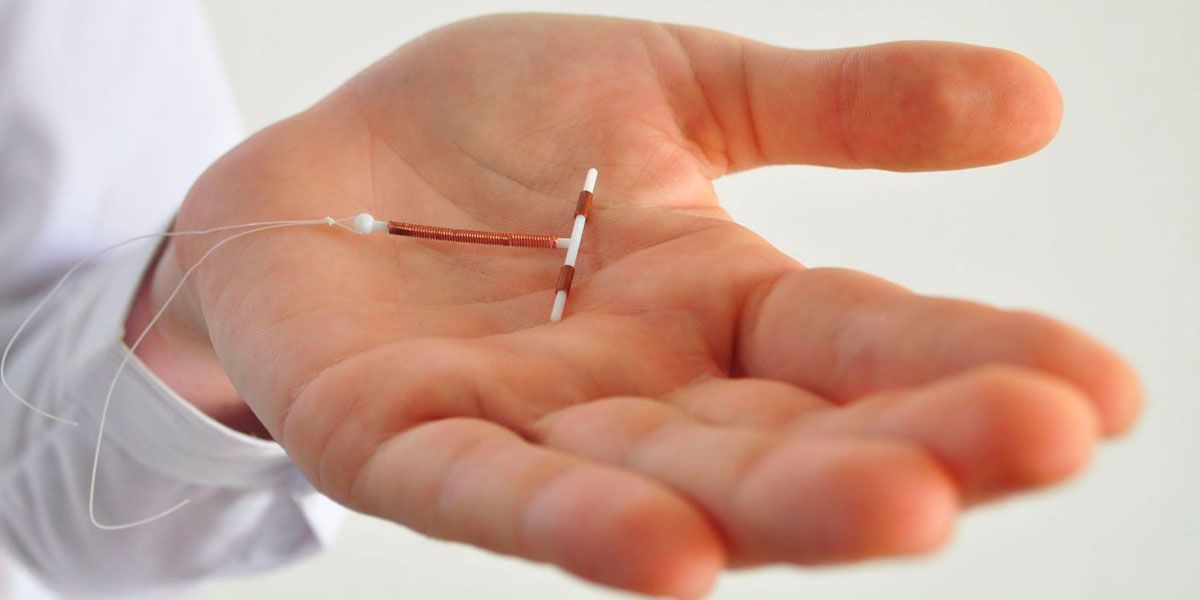
Copper Intrauterine Device (IUD)
Copper Intrauterine Device (IUD)
What is a Copper IUD
An IUD (intrauterine device) is a small plastic device that is inserted into the uterus (womb) to prevent pregnancy. The copper IUD has copper and sometimes silver, wrapped around its stem and arms. It does not contain any hormones. The copper IUD is a highly effective, long-acting reversible contraceptive.
How does it work?
The copper IUD works in the following ways:
the copper is toxic to eggs and sperm which stops an egg being fertilised
it slows the movement of egg and sperm so reduces the chance of them meeting
it...
Hormone Releasing Intrauterine Devices (IUDs)
Hormone Releasing Intrauterine Device
What are hormone-releasing IUDs?
Hormone-releasing intrauterine devices (IUDs) are small plastic devices that are inserted into the uterus (womb) and are used to prevent pregnancy. They contain a hormone called levonorgestrel in the stem. Levonorgestrel is a type of progestogen. A small amount of this hormone is released continuously over a period of time. There are two types of hormone releasing IUDs: the Mirena® and the Kyleena®. The Kyleena® is slightly smaller and releases a lower dose of hormone than the Mirena®.
How do they work?
The...
Condoms
Condoms
What are condoms?
Condoms are worn during sexual activity to prevent sexually transmissible infections and as a contraceptive method to prevent pregnancy. A condom is a physical barrier that stops body fluids (e.g., semen, vaginal fluids) from passing between sexual partners. There are two different kinds of condom available, the external (male) condom and the internal (female) condom.
External (Male) Condoms
What are external condoms made of?
External condoms are made of thin, strong latex rubber or polyurethane.
How do you use them?
They are used by being rolled onto...
Enjoying Sex Safely
Enjoying Sex Safely
What is sex?
Sex can mean different things to different people.
A better way to describe sex would be to say sexual activity, as sex can include a range of things. Sex can include:
Penetration of the vulva/vagina or anus by another person using any part of the body or any object
Contact between a mouth and vulva, penis, or anus
Any other sexual activity that may involve another person / people like kissing and mutual masturbation
Sex is a normal human experience, which should be fun and pleasurable.
What is safe sex?
Safe Sex is not just about taking...
Contraceptive Implant (The Rod)
Contraceptive Implant (The Rod)
What is the contraceptive implant?
The contraceptive implant, often called ‘the rod,’ is a small flexible plastic rod that contains a progestogen hormone called etonogestrel. It is inserted under the skin on the underside of your upper arm, where it slowly releases a small amount of this hormone over 3 years. The contraceptive implant used in Australia is called Implanon NXT.
How does it work?
The contraceptive implant prevents pregnancy by stopping eggs from being released from the ovary (ovulation). It also increases mucus thickness in the cervix,...
Post Natal Contraception
Post Natal Contraception
If there is a chance you will be sexually active and want to avoid pregnancy after you have had your baby, you will need contraception.
Pregnancy can occur from as early as 21 days after birth, so it is important to know what contraception you will be using before this time.
A pregnancy that occurs within 12 months of giving birth can place extra stress on you and your unborn baby and carry more risks of complications, so having effective contraception during this time is particularly important.
Your choice of contraception will depend on many factors, such...
Vasectomy
Vasectomy
A vasectomy is a permanent form of contraception. It iis a minor surgical procedure that involves cutting the 2 small tubes (vas deferens) that carry sperm from the testes to the penis.
After a vasectomy, your semen is the same, but it has no sperm in it.
Vasectomy is a safe, effective, and permanent form of contraception.
How effective is vasectomy?
A vasectomy is over 99% effective.
However, while it is rare, a vasectomy may fail, and you may stay fertile or become fertile again. This can happen if the tubes are not blocked off, grow back together, or if a third tube...
Contraceptive Implant (Implanon NXT) Training Workshop
Contraceptive Implant (Implanon NXT) Training Workshop
Delivered in Canberra, the SHFPACT Contraceptive Implant (Implanon NXT) Training Workshop has been designed for clinicians who wish to learn safe insertion and removal of the contraceptive implant.
This course is open to doctors, nurse practitioners, registered nurses and midwives.
We are a provider of the AUSLARC Scholarships, applications for 2026 are closed.
Learning Outcomes
1. Demonstrate safe insertion of the contraceptive implant
2. Demonstrate safe removal of the contraceptive implant
3. Counsel patients on the use...
Contraception Kits
Contraception kits
SHFPACT hires Contraception Kits to any High Schools and Colleges that have a Friends of SHFPACT Membership (Organisational/Nonprofit/Small Business/Schools).
SHFPACT’s Contraception Kits contain:
1x diaphragm (Caya®)
1x hormone releasing IUD (Mirena®)
6 x male condoms
6 x lubricants
2 x female condoms
2 x dental dam
1 x oral contraception pill sample box
1 x emergency contraception sample box
1 x vaginal ring (Nuvaring®)
1 x contraceptive implant (Implanon®)
1 x contraceptive injection vial in box
1 x demonstrator (to demonstrate condom use)
1 x...
Emergency Contraception
Emergency Contraception
What is emergency contraception?
Emergency contraception (EC) is used after unprotected sex to reduce the risk of pregnancy.
You might use emergency contraception if:
• You had sex and didn’t use any contraception
• A condom broke or slipped off during sex
• You missed one or more of your usual contraceptive pills
• You were sexually assaulted
What kind of emergency contraception is available?
There are two types of emergency contraception available in Australia:
• The emergency contraceptive pills (ECP):
The Levonorgestrel emergency contraceptive...
The Pill
The Pill
What is the combined oral contraceptive pill?
The combined oral contraceptive pill, usually simply called ‘the pill’, is a contraceptive pill taken by mouth which contains 2 hormones, oestrogen, and progestogen. These hormones are similar to the hormones produced by your ovaries.
How does it work?
The pill works by preventing ovulation, which means it stops the ovaries from releasing an egg each month, which in turn means that fertilization cannot occur, and a pregnancy cannot begin.
It also thickens the mucus in your cervix, which makes it harder for sperm to get into the...
Contraceptive Options
Contraceptive Options
What is contraception?
Contraception (also called birth control) protects you from pregnancy. There are a number of different methods of contraception available. It is important to choose a method that suits you.
Using contraception gives you more control, allows you to decide if, and when, to have children, and allows you to enjoy sex without having to worry about an unintended pregnancy.
Which contraceptive is right for me?
Many factors affect your choice of a contraceptive method including:
Your stage of life
Your lifestyle
How effective the method...
IUD Insertion Workshop
IUD Insertion Workshop
This course is suited to experienced GPs, Nurse Practitioners, and Midwives who have a desire to provide IUD insertions for their patients and have at least 10 patients per year who require IUD insertion. May be required to demonstrate evidence of prior contraceptive learning and clinical experience.
We are a provider of the AUSLARC Scholarships, applications for 2026 are closed.
Important Note: Please check eligibility criteria below before applying.
2026 workshops are currently full, if you would like to join the waitlist please email This email address...
The FPAA Certificate Course for Doctors in Reproductive and Sexual Health
Sexual and Reproductive Health Australia National Certificate for Doctors
Nationally Accredited Training for Medical Practitioners
This nationally accredited course is designed for doctors who wish to expand their knowledge and clinical skills in delivering sexual and reproductive healthcare. The program includes a theory and assessment component, with the option to undertake a supervised clinical attachment to complete the full Sexual and Reproductive Health Australia National Certificate for Doctors.
Theory Component
22- 24 May 2026Delivered face-to-face over three consecutive...
The Caya Diaphragm
The Caya Diaphragm
What is a diaphragm?
A diaphragm is a barrier method of contraception. It is a dome of soft silicone with a flexible rim that is placed inside the vagina to cover the cervix (the lower part of the uterus or womb). The Caya® diaphragm, which is a single size diaphragm, is the only one available in Australia.
How does it work?
The diaphragm forms a barrier which prevents sperm from getting into the uterus. It is inserted before sexual intercourse and is left in place for at least 6 hours afterwards. It takes 6 hours for the sperm to die in the acidic environment of...
AUSLARC Scholarships now open
We’re excited to let you know that the AUSLARC Scholarships are now open!
These fully funded scholarships provide training in Implanon and IUD insertion for eligible health professionals, equipping you with the skills to expand contraceptive choice and support reproductive health in your community.
AUSLARC is led by Sexual and Reproductive Health Australia (SRHA) in partnership with the Royal Australian College of General Practitioners (RACGP). This initiative received grant funding from the Australian Government. It includes a national evaluation framework to support long-term impact and...
Sexual and Reproductive Health Australia National Certificate for Doctors Theory Only
Theory Only Sexual and Reproductive Health Australia National Certificate for Doctors
Course Overview
This intensive and in-depth training program is designed for doctors/independent primary care clinicians aiming to deliver high-quality sexual and reproductive healthcare in primary care settings.
This theory course is part of the Sexual and Reproductive Health Australia National for Doctors. We understand Nurse Practitioners and Midwives have a unique Scope of Practice and may benefit from attending the theory component of this certificate.
2026 Course Dates TBC
Theory...














-dd2f751e.png)
