Early Pregnancy Health and Care

Good health and care in pregnancy are essential for you and your baby and are especially important in early pregnancy.
When should I see a doctor?
Ideally, you should see a doctor before you become pregnant to discuss pre pregnancy health and any tests you may need. You can also discuss any medical problems, medications, supplements, and general health in pregnancy.
If this hasn’t happened because your pregnancy was unplanned or unexpected, then when you first find out you are pregnant is an excellent time to visit your GP. They can give you essential information, answer questions, discuss the routine tests you need in early pregnancy, explain options for care in pregnancy, and refer you to whoever will be undertaking your pregnancy care.
How is the length of a pregnancy calculated?
Pregnancy is counted from the first day of your last normal menstrual period and lasts about 40 weeks from that time.
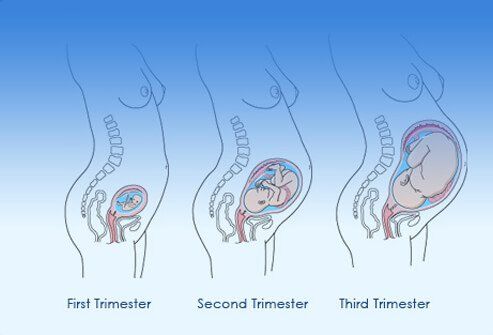
Pregnancy is divided into 3 trimesters:
- First trimester: up to 12 weeks
- Second trimester: 13 to 27 weeks
- Third trimester: 28 to 40 weeks
Health in early pregnancy
Nutrition in pregnancy
Pregnancy places significant demands on your body. Good nutrition during this time is critical for your health and the health of your developing baby.
You only need a slight increase in the amount of food or calories; it is the quality of your diet that really matters. Your need for protein, iron, iodine, and folate increase in pregnancy.However, what is most important is a healthy balanced diet that includes foods from all food groups.
A healthy diet has a high intake of fresh fruit, vegetables, whole grains, proteins such as legumes, eggs, nuts and seeds, tofu, lean meats, fish, and calcium-containing foods such as dairy or calcium-fortified dairy alternatives.
Vegetarian and vegan diets
A vegetarian diet can meet the needs of your pregnancy if you take care to include food from all five food groups daily.
A vegan diet requires more careful planning to make sure it provides the essential nutrients you and your baby need. If you do eat a vegan diet, it is recommended that you see a dietitian for advice.
Multivitamin supplements in pregnancy
There is evidence that taking a mutlivitamin in pregnancy may reduce the risk of a baby being small, the risk of pre-term birth, and of some abnormalities. However, a healthy balanced diet should be adequate for most people. If you do wish to take a multivitamin make sure it is a pregnancy specific multivitamin.
Folate
Folate (also known as folic acid) is one of the B-group vitamins and is critical for your baby's healthy development in early pregnancy. Folate is found naturally in foods such as green leafy vegetables, broccoli, brussel sprouts, oranges, bananas, strawberries, and legumes. However, most people do not eat enough to meet their pregnancy needs, and taking a supplement is always recommended.
Taking 500 micrograms(mcg) of folate daily for at least 4 weeks before conception and during the first 12 weeks of pregnancy is advised. Folate is available in tablet form from pharmacies. If you have certain conditions such as diabetes or epilepsy, a higher dose of folic acid may be recommended for you.
Iodine
Iodine is an essential nutrient for humans. It is especially important for your baby’s developing brain and nervous system during pregnancy and in infancy. Therefore, it is recommended you take an iodine supplement of 150 micrograms(mcg) a day during pregnancy and breastfeeding. Tablets that contain both folate and iodine are available in pharmacies. Talk to your GP about iodine supplementation to make sure that you have no contraindications.
Iron
Iron is an essential nutrient needed to make red blood cells that carry oxygen around your body. Your iron requirements increase during pregnancy and a deficiency can cause tiredness, dizziness, and lower resistance to infection. You can usually get enough iron from eating iron rich foods, which is recommended rather than taking a supplement. However, some people may find that they need iron supplementation, such as those who have a vegetarian or vegan diet, have a history of iron deficiency, or have a multiple pregnancy. Iron supplements can cause side effects, so discuss this with your GP if you think you may need one.

Vitamin D
Vitamin D is a nutrient that helps to maintain bone and muscle strength, and assists you with absorbing calcium. It also helps your baby to develop strong bones. In pregnancy it is recommended that you take a Vitamin D supplement of 400IU a day ot take a pregnancy supplement containing vitamin D.
Vitamin B12
Vitamin B12 is one of the B group vitamins and is essential for the development of your baby's brain and nervous system. It is primarily found in meat, fish, dairy, and eggs. There are people at an increased risk of B12 deficiency, including anyone with a family history of B12 deficiancy, with a condition that affects absorbtion, or if you have a strict vegtarian or vegan diet. In this case, you should consider supplementation with Vitamin B12 in pregnancy and during breastfeeding. B12 is available in tablet form from any pharmacy, or by injection if absorption is a problem. If you feel you are at risk of B12 deficiency, discuss this with your GP.
Calcium
Calcium is an essential mineral and is important during pregnancy and breastfeeding because it is needed for your baby’s bones to form. Calcium supplements are not considered necessary in pregnancy unless advised by your GP. Dairy foods, such as milk, cheese, yoghurt, and calcium-fortified plant-based milk products are excellent sources of calcium. Aim for three serves a day.
Omega-3 fats
Omega- 3 fatty acids are required for the development of your baby's brain, nerves, and eyes. Sources of omega-3 fats include oily fish such as salmon, tuna, and sardines, walknuts, chia seeds, soybean priducts such as tofu, and linseed.
Herbal preparations
There is not enough evidence on the safety or effectiveness of using herbal preparations during pregnancy. Ginger is considered safe and may help to reduce pregnancy-related nausea when taken as tea, lozenges, or chews. You should avoid taking any other herbal preparations in the first trimester. If you are considering taking any herbal preparations other than ginger, please talk to your GP.
Mercury in fish
Fish can be a valuable source of protein and omega-3 fats in pregnancy, and it is recommended to eat fish 2-3 times a week. However, some fish contain mercury which can cause developmental delays in children exposed in pregnancy. It's best to avoid fish that may contain a higher level of mercury. Fish that contain higher levels of mercury include flake, ray, swordfish, barramundi, gemfish, orange roughy, ling, and southern blue fin tuna.
Water
Your need for water increases significantly during pregnancy, so it is essential to make sure that you are drinking plenty of water every day. If you are having difficulty drinking due to morning sickness, try sipping small quantities of water or clear non-caffeinated fluids like lemonade or apple juice frequently throughout the day.

Caffeine
While there is no clear evidence of harm from consuming caffeine in pregnancy, some studies have linked high caffeine consumption with miscarriage and low birth weight in babies. Low to moderate caffeine consumption (up to 3 cups of coffee or 6 cups of tea a day) is considered safe in pregnancy. Be aware that cola drinks contain caffeine too. Energy drinks have a high caffeine content and should be avoided.
Weight gain in pregnancy
Weight gain in pregnancy is very normal, and is due to changes in your body tissue, increase in the size of your breasts and uterus, increases in fluid and blood volume, and the weight of your developing baby.
Weight gain varies between individuals. Average weight gain is usually between 11 and 16 kilos. Most pregnant people gain around 1 to 2 kilos in the first 3 months, and 1 to 2 kilos a month for the last 6 months. It is important not to try to lose weight in pregnancy as this can affect the health of the baby, however gaining too much weight can also cause health problems for you. If you are concerned about weight, discuss this with your GP or with a dietician.
If you are underweight,(BMI less than 18.5) having extra serves of the five food groups may contribute to healthy weight gain.
If you are overweight or obese (BMI 25-29.9 or over 30) limiting serves and avoiding energy-dense foods may limit excessive weight gain. Weight-loss diets are not recommended during pregnancy.
Food safety in pregnancy
Your immunity is lower in pregnancy and there is a slightly increased risk of developing a foodborne illness which can be dangerous for your baby. It is important to take steps to reduce the risk of becoming infected.
Avoiding foodborne illnesses during pregnancy
- Eat freshly prepared and cooked foods
- Practise good food and hand hygiene such as regular handwashing, washing fuit and vegetables before eating or cooking, keeping surfaces and cutting boards and implements clean, and keeping raw meat seperate from other foods.
- Foods to avoid
- chilled seafood such as smoked salmon, mussels, oysters. prawns, or raw seafood such as sushi.
- pre-pared or pre-packaged food from buffets, salad bars, and sandwich bars.
- deli meats such as pate, ham, salami, or pre-cooked and diced chicken.
- undercooked meat or poultry.
- unpasteurised milk or foods made from unpasteurised milk.
- soft-serve ice creams.
- soft cheeses, such as brie, camembert, ricotta, and feta.
- ready-to-eat foods, including leftover meats, which have been refrigerated for more than one day.
- dips, and salad dressings in which vegetables may have been dipped.
- pre-cut and pre-packaged vegetables or fruit or make sure you cook them before eating.
- raw or lightly cooked sprouts.
- raw eggs or products made witg raw eggs, such as mayonnaise or aioli.
Cytomegalovirus (CMV)
This is a common virus with about 50% of adults having been infected. It is often found in toddlers and young children. CMV infection is usually mild but can be dangerous for unborn babies if the mother is infected in pregnancy. Transmission can be reduced with simple hygiene measures such as washing hands often, especially before and after preparing food, and after going to the toilet; practising good hygiene during nappy changes; washing toys; avoiding contact with child's saliva; and not sharing food, drinks, or eating utensils.
Toxoplasmosis
This is a parasite typically found in birds and mammals (including cats). You can also be exposed from sources such as raw meat and shellfish, as well as soil, water, and plants. Infection during pregnancy can cause congenital disabilities in babies. To reduce the risk of exposure avoid close contact with cats, do not change litter trays, wear gloves during gardening, avoid uncovered sanpits where you might find cat faeces, avoid any raw meat or seafood, and follow the guidelines for avoiding food-borne illnesses above.
Physical activity in early pregnancy
Physical activity is beneficial throughout life, including in pregancy, All pregnant women who do not havecontraindications should aim to meet the recommended physical activity for adults.
It is advisable to avoid any physical activity that may risk a fall, any abdominal trauma, or excessive strain on your joints. These include high-impact sports and contact sports. Scuba diving is also not advised. If you have any physical problems or conditions that may interfere with exercising always discuss it with your GP or midwife first.
Medications/drugs
While some medications are quite safe to use in pregnancy, there are medications and prescription drugs that can be harmful to unborn babies. Discuss any prescription medications with your doctor if you are thinking of becoming pregnant, or as soon as you are pregnant. It is important not to stop any prescribed medications without consulting your doctor first.
Do not take any over-the-counter medications without checking with your doctor, pharmacist, or midwife. This includes common drugs such as aspirin or ibuprofen, as well as any complementary or herbal medicines. It is usually better to avoid taking any non-essential medication; however, some medications such as antibiotics are necessary and safe options can be prescribed.
Vaccinations in pregnancy
There are some vaccinations that are advised in pregnanct, and others that need to be avoided or delayed. Vaccinations that are safe and advised in pregnancy include COVID-19, infuenza, pertussis (whopping cough), and RSV. You will need to discuss any possible vaccinations with your GP.
Alcohol
Alcohol consumed during pregnancy passes directly into your unborn baby’s blood supply. It can have severe effects on an unborn baby and can result in a condition called foetal alcohol spectrum disorder (FASD), which has a range of serious physical, behavioural, and mental effects that are lifelong. There are no known safe levels of alcohol in pregnancy, so it is advised that you avoid drinking any alcohol during pregnancy or when you are planning pregnancy.
Illicit drugs
Many illicit drugs can seriously affect your baby’s health if used during pregnancy. These include marijuana, MDMA, cocaine, amphetamines, LSD, and heroin. It is best to avoid all drugs during pregnancy. However, if you are using any drugs be sure to talk to your GP or midwife. They can put supports in place for you or link you to services that can help you and your baby stay as healthy and as safe as possible.
Smoking and vaping
It is well known that smoking causes serious harm to you and your developing baby. This includes passive smoking, where someone is exposed to another person’s smoking. Smoking in pregnancy can cause complications and is linked with pre-term birth, a baby having a low birth weight, being small for age, birth abnormalities, and even an increased risk of miscarriage, stillbirth, and SIDS.
There is limited evidence available on the health effects of vaping during pregnancy, however, there are indications that it increases the rate of preterm birth. Vaping also exposes you and your baby to numerous toxic chemicals that may cause additional health risks.
The sooner that you stop smoking in pregnancy the better for you and your baby.
Talk to your GP about getting help to stop or reduce smoking or call the QUITLINE on 137 848.
Environmental toxins
Some common substances are known to be potentially toxic during pregnancy and are best avoided completely, these include dry cleaning products, oven cleaners, paint thinners or paint strippers, insecticides, herbicides, and any products or materials which may contain lead or mercury. If you are uncertain about a substance, then it is best to avoid it.
Morning sickness
Morning sickness during pregnancy is common. Symptoms include loss of appetite, aversions to certain foods and smells, retching, nausea, and vomiting. Despite its name, morning sickness can occur any time of the day or night.
It usually resolves by 16 to 20 weeks of pregnancy. Things that may help lessen the effects of morning sickness:
- Avoid an empty stomach. You can do this by eating small frequent meals, eating a few dry crackers before getting out of bed in the morning, and keeping light snacks to eat with you during the day.
- Avoid rich, fatty, or spicy foods.
- The use of ginger (chew, lozenges, capsules, or tea) may be helpful and is considered safe in pregnancy.
- Some women find the use of acupressure helpful.
There is some evidence that iron supplements and multivitamin supplements containing iron may worsen nausea and vomiting. Discuss this with your GP or midwife.
Prescription medications are available that are considered safe to use in pregnancy to help reduce morning sickness.
If your morning sickness is becoming difficult to manage or you experience persistent vomiting, see your GP.
Travel in pregnancy
Car travel
Seat belt use reduces the risk of serious outcomes for you and your baby in the event of an accident. Therefore, it is important that you always wear a seatbelt, making sure the straps are placed above and below the bump, not over the bump.
Air travel
Air travel before 36 weeks of pregnancy is allowed by most airlines. Some airlines may require a letter from your doctor or midwife. The risk of blood clots increases in pregnancy and as air travel also increases the risk of blood clots, take the usual precautions of moving about when you can, staying well hydrated, and using support stockings to reduce this risk. Make sure you wear your seat belt under the bump.
Overseas travel
Immunity is lower in pregnancy. Therefore, there is a slightly increased risk of developing a food-borne illness that can be harmful to your baby. Caution should be used when travelling to countries with a high rate of food-borne illnesses.
Anti-malaria medication is not safe during pregnancy, so travel to malaria-endemic countries is not advised if you are pregnant. If travel to these areas is unavoidable, then other precautions should be taken to avoid bites from malaria-carrying mosquitoes. Discuss this with your doctor or a specialist travel clinic.
Travel vaccines
Some travel vaccinations are not safe to use in pregnancy. Discuss this with your GP or specialist travel doctor id you plan to travel to a country where vaccination is advised.
Travel insurance
If you are traveling when pregnant make sure that you have travel insurance. Any travel insurance policy you purchase needs to cover you for pregnancy, and for pregnancy or birth complications.
Sex in Pregnancy
Sexual activity in pregnancy is considered quite safe if there are no complications with the pregnancy. Libido in pregnancy is quite individual; some people’s interest in sex decreases, but it may be unchanged or even increase for others. It is common for interest in sex to decline as the pregnancy progresses.
Mental Health
Pregnancy and the experience of pregnancy is individual for everyone. Some people find that their mental health remains unchanged or that they may even feel calmer than usual during pregnancy. However, some people experience increased anxiety and/or depression during pregnancy or in the post-natal period. If you have had mental health concerns before pregnancy then your risk of developing a problem during pregnancy is slightly increased.
If you have concerns about this or feel that you are experiencing some changes to your mood or to your level of anxiety, it is very important to discuss this early with your GP or midwife. There is good support available.
- Canberra Health Services runs a support line for anyone who needs support in pregnancy, Early Pregnancy Support: Call 02 5124 1775.
- Perinatal and infant Mental Health. This is a free service run by Canberra Health Services for people who are pregnant or have a baby under 12 months and have a severe mental health problem. Your GP or midwife can refer you or you can also self-refer by calling 02 5124 3133 between 10am to 4pm Monday to Friday.
- The Perinatal Wellbeing Centre is a non-government organisation supported by ACT Health that provides individual and group mental health support to people in pregnancy and after birth until your youngest child is 2. The service is free, and you do not need a referral. To access this service call 02 62881936.
- If you are a client of Mental Health ACT or receiving opioid replacement there is a special service called the IMPACT Program that can assist you with managing your care in pregnancy. You Gp can refer or you can access the service by phone on 1800 211 274 from 9:00am to 4.30 pm weekdays.
- There are also some private psychologists who specialise in perinatal mental health.
If you have a serious diagnosed mental health issue such as bipolar disorder, borderline personality disorder, schizophrenia, or major depressive disorder it is essential that you receive appropriate care and support during your pregnancy. Talk to your GP, midwife, or your mental health professional about your pregnancy and the support services available for you.

Higher risk pregnancies
People may sometimes need specialised care in pregnancy. If you have a serious medical condition or have had a previous pregnancy affected by blood clots, pre-eclampsia(high blood pressure), pre-term birth, or a previous still birth you are considered at higher risk in your next pregnancy and are advised to see your GP early so that appropriate care can be arranged.
Pregnancy & birth care
Pregnancy care and birthing options
Care during pregnancy is called antenatal care. Regular antenatal care is important for your health and the health and wellbeing of your baby.
Your GP, midwives, an obstetrician, or a combination of these can provide antenatal care. The recommended number of visits for antenatal care during pregnancy is eight to ten.
Your first antenatal visit should include:
- a family history,
- a medical check, including routine blood tests
- a discussion about your pregnancy and birth care
- discussions about tests in pregnancy
It is a good idea to start thinking about the kind of care you want to receive during pregnancy and birth as soon as possible and to discuss this with your GP. There are several choices available in the ACT.
Models of care include midwife-led continuity of care programs (available through the Centenary Hospital for Women and Children or North Canberra Hospital) or care with a private obstetrician. In addition, specialist care is available for higher risk pregnancies.
There is also a publicly funded homebirth service for those who meet the criteria, and private homebirth midwives.
If you have private health insurance and are considering seeing a private obstetrician, make sure your plan covers pregnancy and delivery.
For more information on pregnancy care and birthing options in the ACT see the websites below.
Early pregnancy information and birth education classes
Most hospitals offer free antenatal and birth education classes to provide you with current information and education about pregnancy, birth, and breastfeeding. There are also private classes available.
For more information see: Having a Baby in Canberra and ACT Health: Pregnancy and Birth.
For more information on birth options, classes and education in Canberra vist Having a Baby in Canberra
What should I do next?
The next step is to make an appointment to see your GP, or find a GP if you don’t have one.
If you wish to access public maternity care, see ACT Health's website: Now you are pregnant or call 5124 9977 to make an appointment with a midwife to discuss your options. This appointment will occure after you are ten weeks pregnant.
Recommended Websites
For reliable evidence-based health information on pregnancy, birth and beyond see: