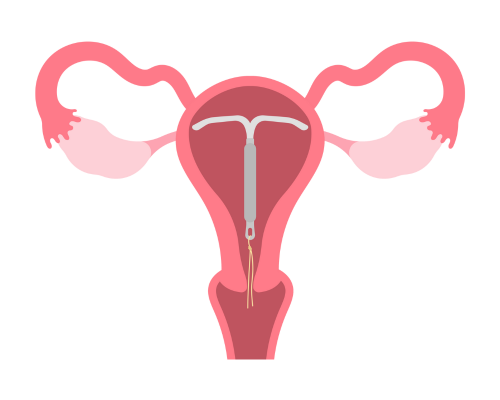
Hormone Releasing Intrauterine Device

What are hormone-releasing IUDs?
Hormone-releasing intrauterine devices (IUDs) are small plastic devices that are inserted into the uterus (womb) and are used to prevent pregnancy. They contain a hormone called levonorgestrel in the stem. Levonorgestrel is a type of progestogen. A small amount of this hormone is released continuously over a period of time. There are two types of hormone releasing IUDs: the Mirena® and the Kyleena®. The Kyleena® is slightly smaller and releases a lower dose of hormone than the Mirena®.
How do they work?
The hormone-releasing IUDs work mainly in the uterus (womb) by preventing fertilisation. They do this by:
- thickening the mucus in the cervix to prevent sperm entering the uterus
- interfering with sperm movement
- thinning the lining of the uterus.
The Mirena® IUD can also be used to assist in the control of heavy menstrual bleeding and can form part of menopause hormone therapy (MHT).
How effective are they?
The hormone-releasing IUDs are over 99% effective at preventing pregnancy.
How long do they last?
- The Mirena® lasts up to 8 years when used for contraception. When the Mirena is used for other reasons (such as heavy menstrual bleeding or as part of menopause hormone therapy), then the time it is used for may be different, so please discuss this with your doctor.
- The Kyleena® lasts for 5 years.
What are the advantages of hormone-releasing IUDs?
- They are highly effective contraceptives
- They do not require any day-to-day action on your part
- They are long-acting (5 to 8 years, depending on the type)
- The contraceptive effect stops as soon as you have the IUD removed
- They are suitable regardless of whether you have given birth or not
- They are a very cost-effective method over time
- As with most contraception, they can be used when breastfeeding
- Both the hormonal IUDs decrease menstrual bleeding and pain (it is common to have very light or no periods)
- The Mirena® IUD can be used to manage heavy menstrual bleeding
What are the disadvantages of hormone-releasing IUDs?
- They must be inserted and removed by a specially trained doctor or nurse
- As with any procedure, there is always a small risk of complications
- The insertion procedure can be uncomfortable or painful
- They do not provide protection from sexually transmissible infections (STIs)
- It is common to experience light bleeding and spotting for 3 to 6 months after insertion
- Your periods may be irregular, and some occasional light spotting can continue longer-term
- Some people may have differences in their bodies that prevent them from having an IUD inserted
Who cannot use a hormone-releasing IUD?
The hormone-releasing IUDs are suitable for most people with a uterus. However, they may not be suitable for you if:
- you think you might be pregnant
- you have had a recent infection of your pelvic area (pelvic inflammatory disease)
- you have unexplained bleeding from your vagina
What are the possible problems which may occur with hormone-releasing IUDs?
- Pregnancy: There is a small risk of pregnancy occurring with hormone-releasing IUDs (less than 1 in 100). However, if pregnancy does occur, there is a slightly increased risk of it occurring in the fallopian tube (this is called an ectopic pregnancy).
- Infection: There is a small risk of infection at the time of insertion (about 1 in 500).
- Expulsion: In about 5% of cases, the uterus will expel (push out) the device. You need to check that the IUD is still in place by feeling for the IUD string at the upper end of the vagina after each period. If the string is not there, it might mean that the IUD has moved or been expelled.
- Perforation: This is a rare event (approximately 2 in 1,000 insertions) that occurs when the IUD passes through the wall of the uterus into the pelvic area. It requires surgery under a general anaesthetic to remove the IUD.
- Other: Some people report weight changes, reduced desire for sex, and mood changes, however; there is currently no scientific evidence to show that the hormone-releasing IUDs cause these effects, and other aspects of life may be contributing factors.
How is a hormone-releasing IUD inserted?
A specially trained doctor or nurse inserts the hormone-releasing IUD. It involves inserting a small device called a speculum into the vagina, then using a special IUD inserting tube to place the IUD into the uterus.
Insertion is done using local anaesthetic at SHFPACT. We are unable to offer insertion under sedation. If you would like to have your IUD insertion under sedation, some clinics do provide this service; please ask our staff about this.
How is an IUD removed?
A specially trained doctor or nurse can remove a hormone-releasing IUD. It is a relatively quick and straightforward procedure.
Where can I have a hormone-releasing IUD inserted?
IUDs need to be inserted by a doctor or nurse with specialised training. The clinic at SHFPACT provides IUD insertion services with doctors. Some GPs and most gynaecologists also offer this service.
What happens when I have a hormone-releasing IUD inserted at SHFPACT?
First appointment
- You will need a first appointment with a doctor to see if a hormone-releasing IUD is right for you.
- At this appointment, the doctor will discuss the IUD and explain the insertion procedure. You may also need a vaginal examination at this time.
- This is an excellent time to ask any questions or raise concerns.
- You will be given a prescription for the IUD. You will need to go to the chemist and have this filled; then, you need to bring the IUD with you at the time of your insertion appointment.
- The doctor will discuss the best timing for your insertion with you, taking into consideration your menstrual cycle and what contraceptive you might be using currently.
- Following your first appointment, you need to make an appointment for the insertion.
Insertion appointment
- You need to bring your hormone-releasing IUD with you to your insertion appointment.
- You will be at the clinic from 1 to 1 ½ hours. If parking, please ensure you leave enough time.
- The doctor will talk with you about the procedure and make sure the process is clear.
- You will be asked to go behind the screen, remove your clothes from the waist down, and lay on the examination table. There will be a privacy sheet for you to use.
- The doctor will do a quick vaginal examination, then a small device called a speculum will be inserted into the vagina. The IUD will then be put into the uterus using a special inserting tube, then the speculum is removed.
- An uncomplicated insertion procedure takes about 15 minutes.
- A nurse will also be with you throughout the procedure.
- You will be asked to stay at the clinic for at least 20 minutes following the procedure. If you are not feeling well, you will need to stay at the clinic until the staff caring for you think you are well enough to leave.
Will the IUD insertion be uncomfortable?
- The IUD insertion procedure can be uncomfortable for some people and can be quite painful for a small number of people (15%). The pain is similar to bad period pain.
- It is recommended that you take oral pain relief (2 paracetamol and 2 ibuprofen) an hour before your appointment.
- While we offer local anaesthetic to numb the cervix at the time of insertion and can provide an anti-anxiety medication beforehand if needed, we are unable to provide sedation at SHFPACT.
- If you would like to have your IUD insertion under sedation, some clinics do provide this service so please ask our staff about this option.
- A few people may feel faint or nauseous following the procedure. If this happens, you may be asked to remain at the clinic longer.
- If you are concerned about possible discomfort please discuss this with the doctor during your initial appointment
After your IUD insertion
- You will be encouraged to arrange to be driven home and to rest up after the procedure for the remainder of the day. You may need to organise care for children, time off work, etc. The doctor will give you a medical certificate if you need one.
- You will probably be okay returning to normal activities the following day.
- There may be cramping and bleeding in the first few days afterward.
- We advise that nothing should enter the vagina for 72 hours afterward to reduce infection risk– no tampons, no vaginal sexual activity, no water (showering is okay).
- No further appointment is needed unless you are experiencing problems. Your doctor will discuss this with you at the time of your insertion.
You should contact the doctor if:
- You suspect you might be pregnant.
- You experience excessive pelvic pain or tenderness, fever or chills, offensive discharge, or deep pain during sex.
- You can’t feel the string, or you can feel the plastic of the device.
References
- Contraception: An Australian clinical practice handbook 4th Edition.
- Contraception: Intrauterine Devices/ Family Planning QLD
- Hormone-Releasing IUD (Mirena) Fact sheet, Family Planning NSW.
- Contraception: Your questions answered. 6th Edition. Churchill Livingstone, Guillebaud, J & MacGregor, A. 2013.
- TGA